Your Body After COVID-19 Virus or a Chest Infection
Learn How to Manage your Body After a Virus

When your COVID-19, virus or chest infection symptoms are at their worst, you are solely focused on the basics: resting, hydrating and monitoring yourself for worsening symptoms.
However as you're on the road to recovery and your symptoms subside, you can be left feeling flat, and possibly with a dry cough or shortness of breath. In fact it's not always just your chest and throat that are affected. There are many secondary symptoms that come with persistent coughs and sneezes, here are a few that your physiotherapist can help with.
PELVIC FLOOR WEAKNESS
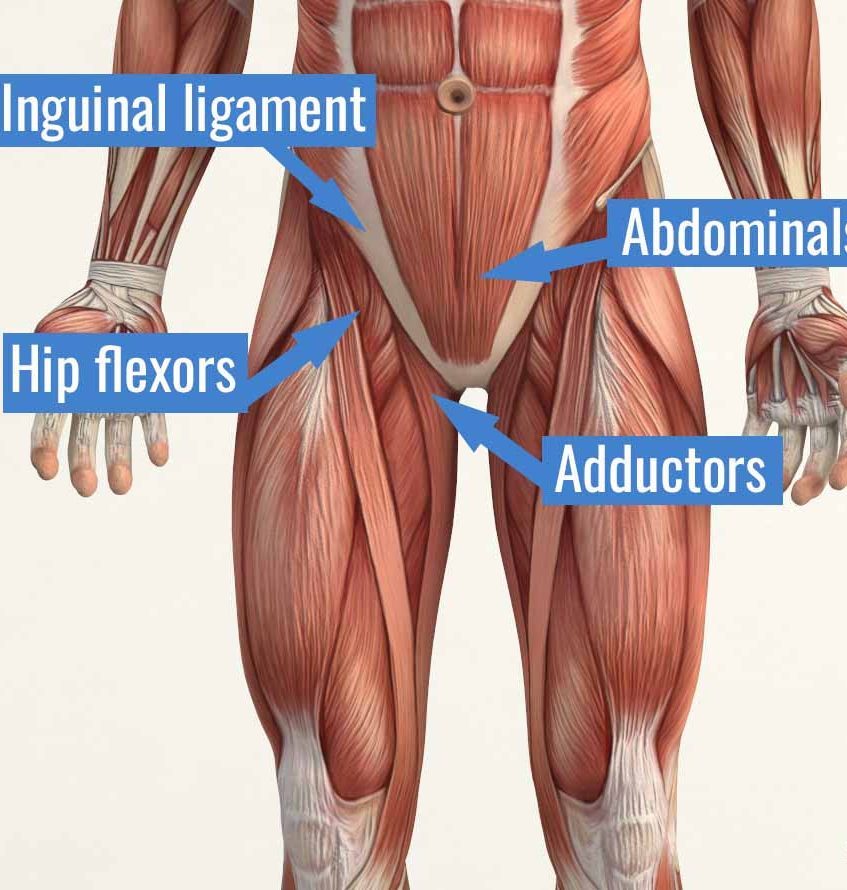
Prolonged coughing can put additional pressure through your abdomen and pelvic floor, which can be a problem if you don't have very good strength to start with. If sneezes and coughs are starting to leave you with a little leakage, know that this is very often treatable. Many physiotherapists specialise in pelvic floor control and strengthening. Doing some basic pelvic floor muscle strengthening, even when you're resting lying or sitting, will help to prevent or improve incontinence. But speak with your physio if you are unsure as to how to do these effectively. We can also use Real Time Ultrasound to help educate you on how to use and activate these muscles. Click HERE to read more about this.
Pelvic floor exercises begin with learning to simply activate the pelvic floor muscles. Here's how you do it...
- The first step is to find a comfortable position, attempt to relax all muscles, and focus on a steady breathing pattern.
- To activate the anterior pelvic floor muscles, replicate the action of stopping the flow of urine mid-stream.
- To activate the posterior pelvic floor muscles, replicate the action of stopping passing gas.
- To activate both the anterior and posterior pelvic floor muscles, combine the two above actions.
When activating the anterior pelvic floor muscles, it is important to not actually stop the flow of urine mid-stream when using the bathroom, as this may lead to difficulty with fully emptying the bladder.
HEADACHES
Coughing and sneezing can raise your ICP (Intracranial Pressure), the pressure of blood on the cranial circulatory system. This can cause a throbbing feeling in your head when feeling unwell. Coughing elevates this pressure, resulting in increased feelings of heaviness and aching. You may also find that coughing and sneezing bring your head into a forward position, putting additional pressure on the muscles at the base of the skull, the most common culprits in causing headaches. Your physio can help you with neck exercises, stretches and postural re-education to help ease these symptoms.
BACK PAIN
Coughing and sneezing also put pressure on your lower back and ribs. If you already suffer from back pain, this might be obvious to you. Many people experience an episode of acute low back pain during or after a chest infection or virus thanks to a sudden, awkward cough. Sneezes in particular create a sudden force on your body that can lead to strains and sprains of the ligaments and muscles around the spine. Your physio can help you with back exercises, stretches and back care tips to help ease these symptoms.
GENERAL ACHES AND PAINS
When your body is in a heightened immune state while fighting an infection, your entire body can feel stiff and achey. Any pre-existing pains can be more painful, particularly neck and thoracic pain. Your physio can help with stretching exercises and advise about return to exercise and sport.
BREATHING
Breathing can be impacted during the acute phases of the virus and beyond. Learning to use your Diaphragm muscle can be a valueable tool to managing this. By doing some regular slow & controlled diaphragmatic breathing you not only get your breathing under control, but you can keep your chest clear, keep your oxygen intake (saturation) high and take the load off your upper shoulders and neck, which can be overused when you're not breathing effectively. Overall you also get more relaxation through your body, which is crucial as you are recovering from any illness.
Here's how you do it....
- Lie on your back on a flat surface (or in bed) with your knees bent. You can use a pillow under your head and your knees for support if that's more comfortable.
- Place one hand on your upper chest and the other on your belly, just below your rib cage.
- Breathe in slowly through your nose, letting the air in deeply, towards your lower belly. The hand on your chest should remain still, while the one on your belly should rise.
- Tighten your abdominal muscles and let them fall inward as you exhale through pursed lips. The hand on your belly should move down to its original position.
You can also practice this sitting in a chair, with your knees bent and your shoulders, head, and neck relaxed. Practice for five to 10 minutes, several times a day if possible.
A colleague and friend who works on the COVID ward at the Royal Adelaide Hospital also advised that improvements are being seen in patients' oxygen saturation levels by changing position, from lying face up to face down. Changing your body position in bed is important to change the airflow in the lungs. If you are short of breath lying down then sit up and practice the above.
EXERCISE
The two muscle groups you can work whilst you're resting are your PELVIC FLOOR and DIAPHRAGM muscles as detailed above. Any other exercise should be commenced GENTLY and GRADUALLY.
When can I start exercising again?
Exercise is an important part of recovering from COVID-19. If your symptoms were mild, you can start exercising again if:
-you’ve had 10 days of rest since symptoms started
-you’ve had at least 7 days with no symptoms, and
-you’re no longer taking any medications such as paracetamol
Start with 15 minutes of light activity like walking or cycling, and see how you feel. Continue to slowly increase the duration and intensity of your exercise, paying careful attention to your heart rate and breathing rate.
Stop exercising immediately and contact your healthcare provider if you have any:
-chest pain or palpitations. If you experience severe central crushing chest pain lasting more than 10 minutes call 000
-unexpected breathlessness
-signs of blood clotting, such as swollen calves.
If you’re recovering from moderate or severe illness, speak with your healthcare provider before returning to exercise.
This article is not intended to replace medical advice. Speak to your physiotherapist or medical pracitioner for more information on how physiotherapy care might be able to help you.